To see what matters.

In the healthcare industry, denials prevention are manual and arbitrary and net revenue projection are built on brittle models, at best.
The time wasted building "timely" reports and solving denials keeps your team from strategically moving the needle on reimbursement. And to make matters worse still, predicting revenue based on unadjusted, billed charges and broad payer reimbursement windows lead to poor financial performance.

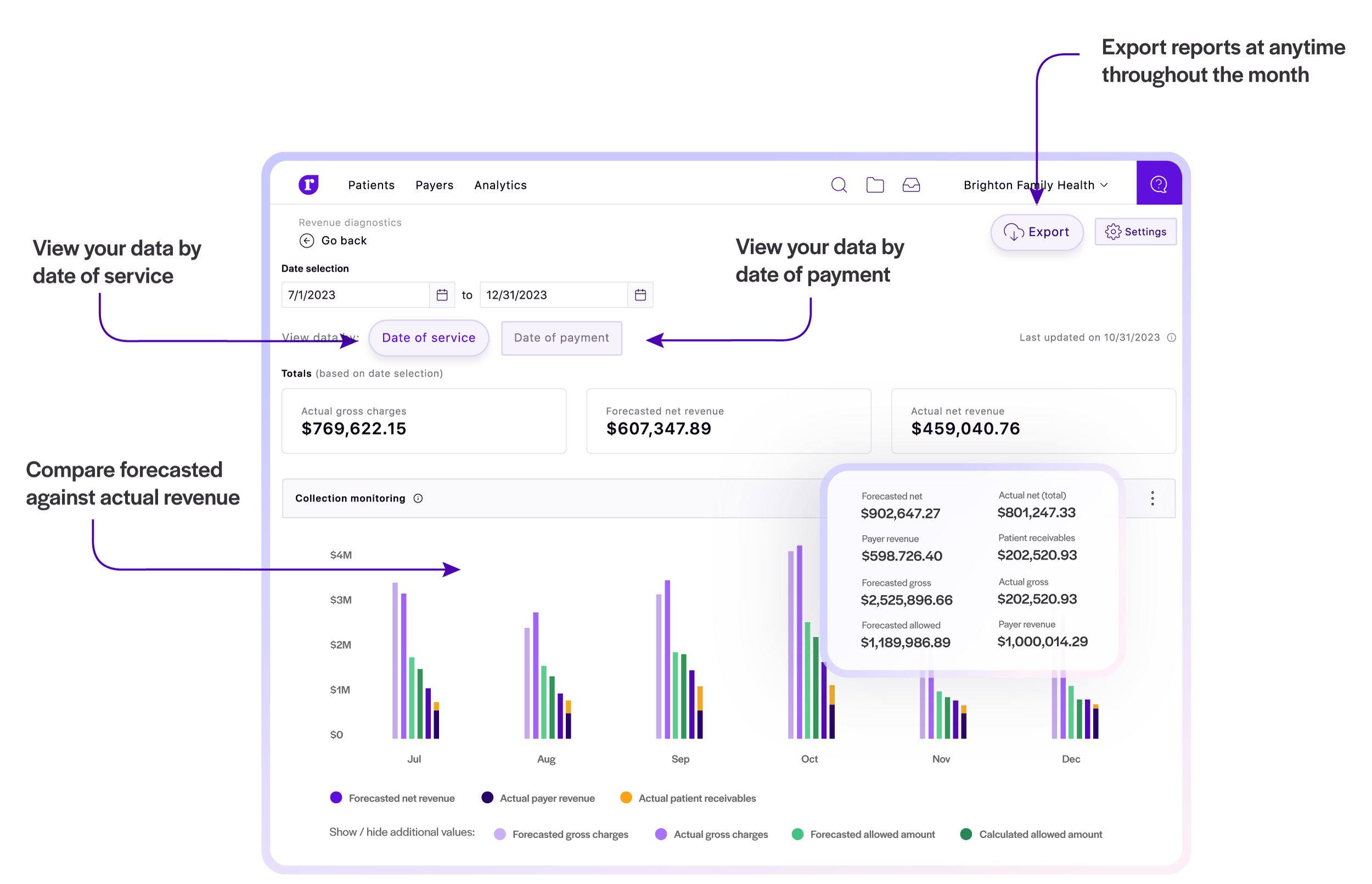
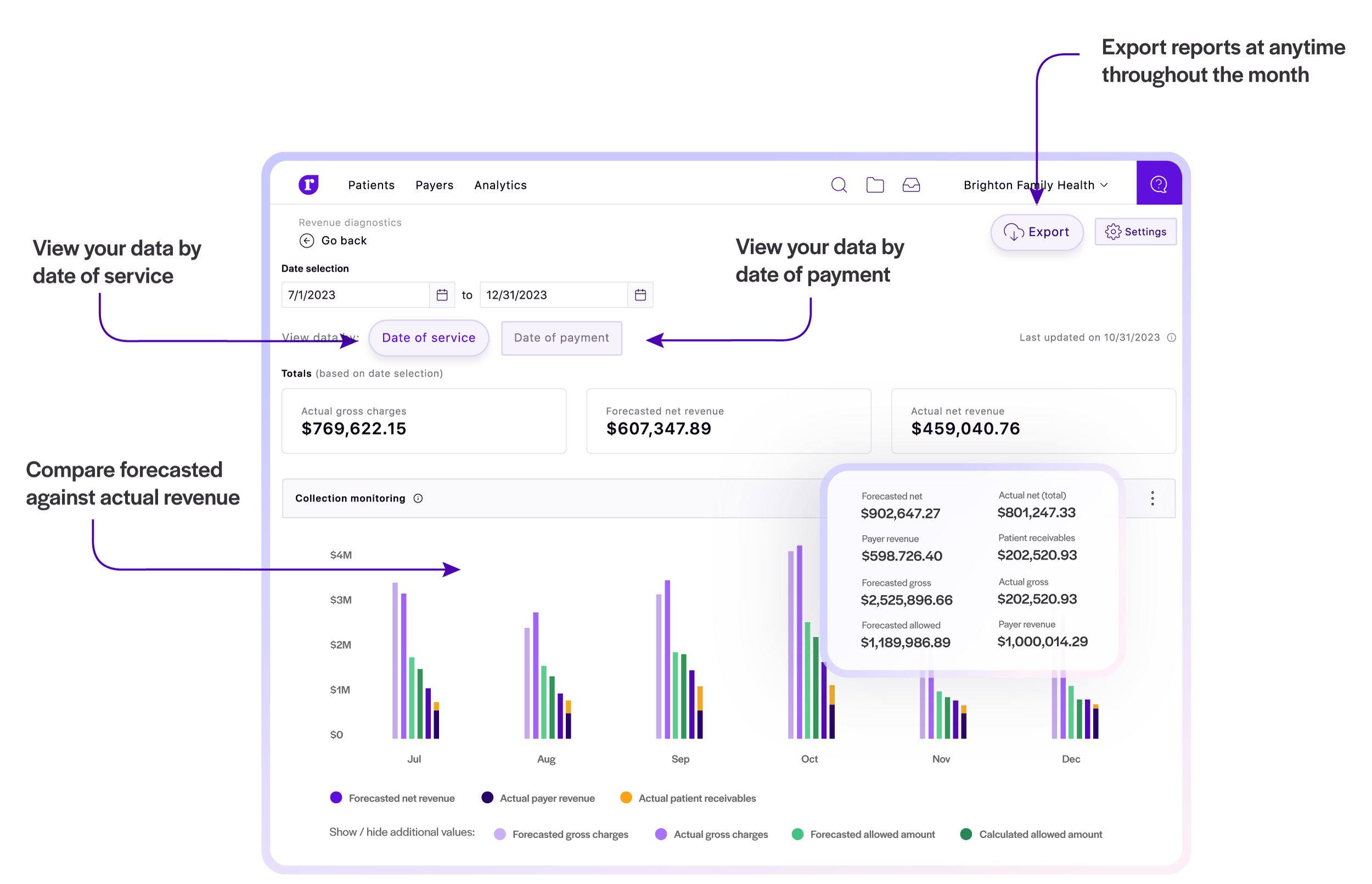
Whether you calculate net revenue and cash by accrual-based or modified cash standards, Rivet is the revenue analytics solution that helps you forecast net revenue with the granularity to confidently gain full visibility of the financial health of your healthcare organization, stop revenue leakage from denied claims with suggestions to avoid payer auto denial, and pursue strategic growth opportunities.
Dive into flexible, responsive dashboards that use artificial intelligence algorithms to show how your claim processes affect your bottom line. Plan your next successful strategic initiative with Rivet at your side.
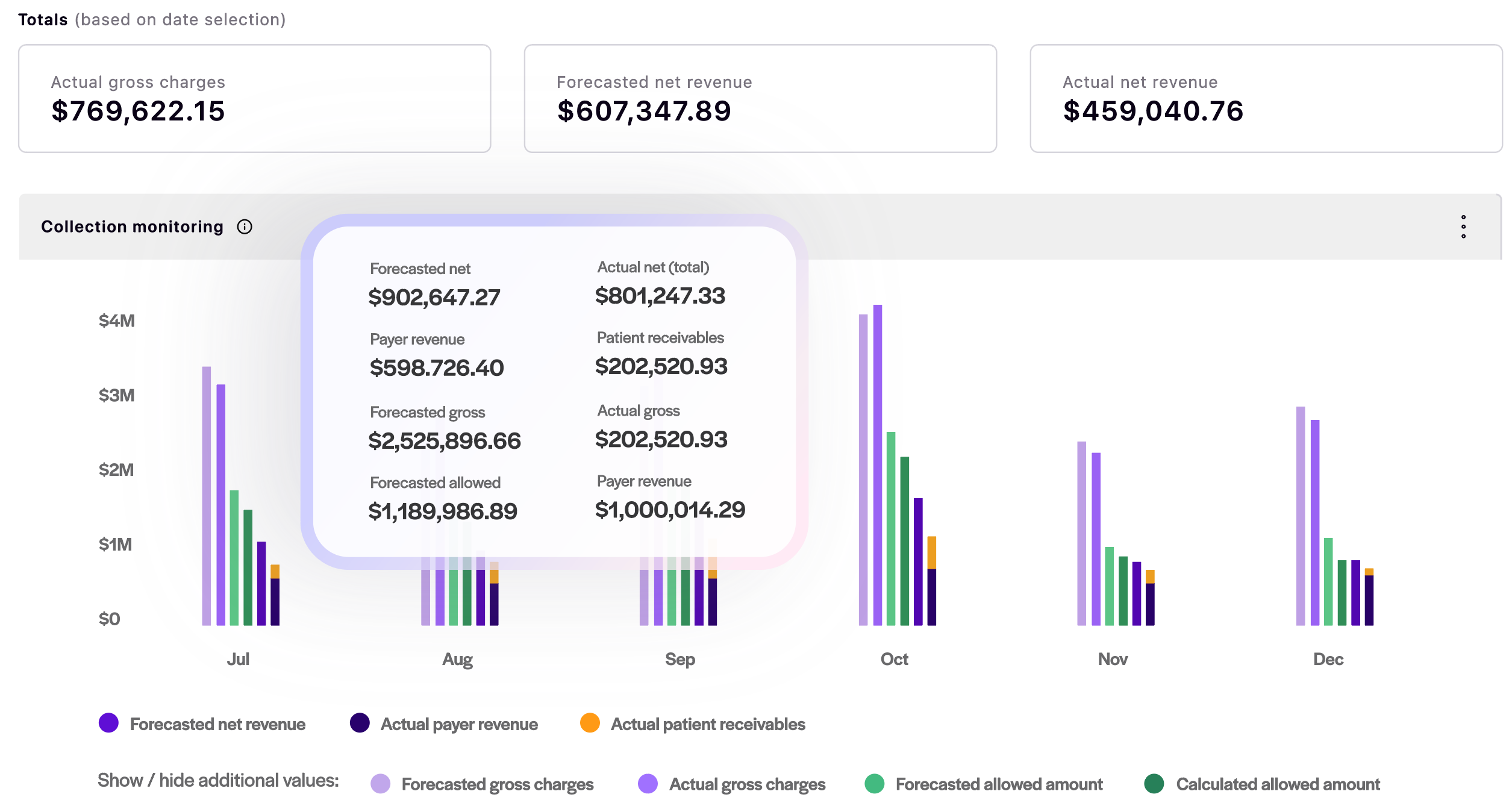
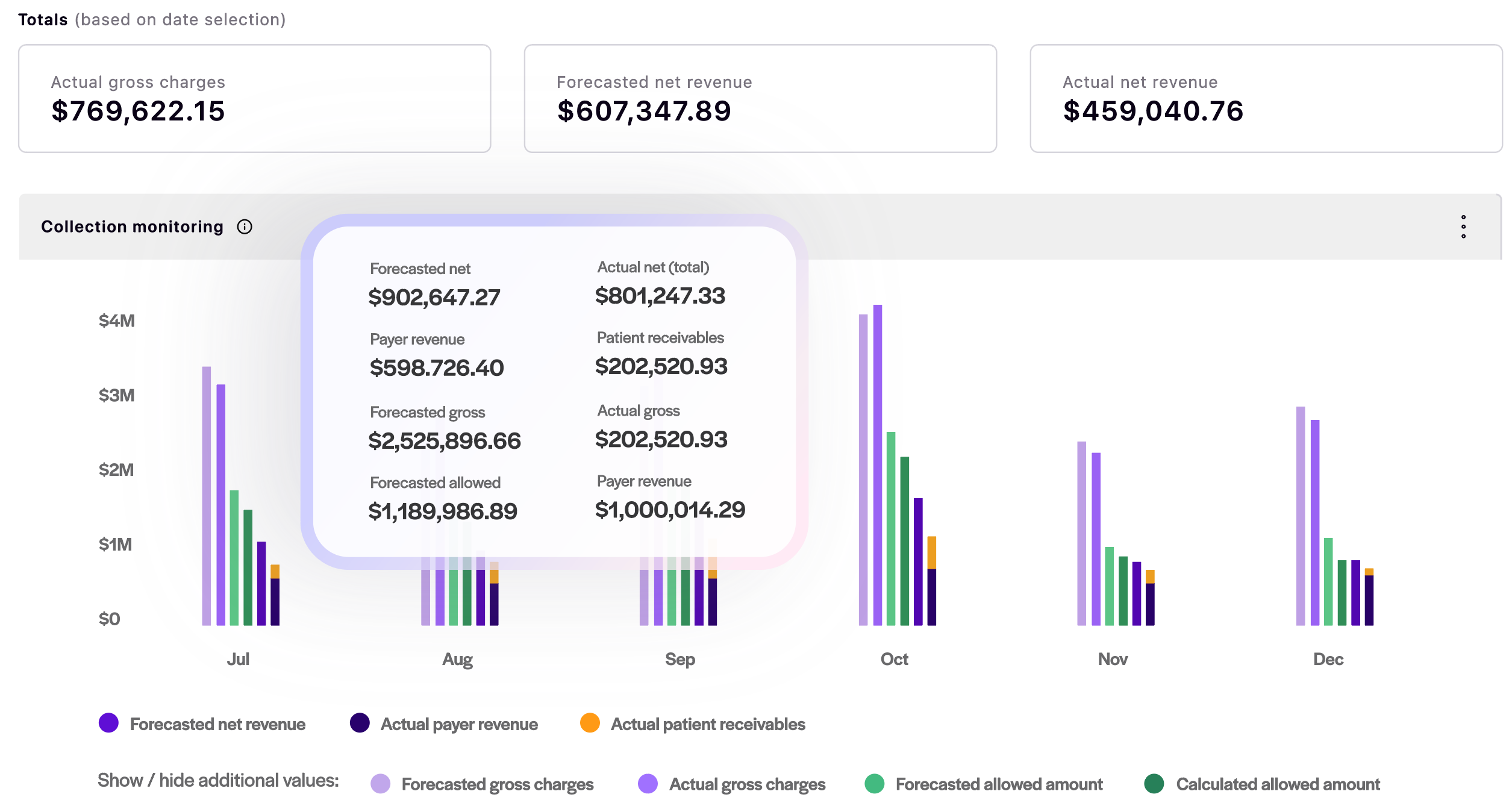
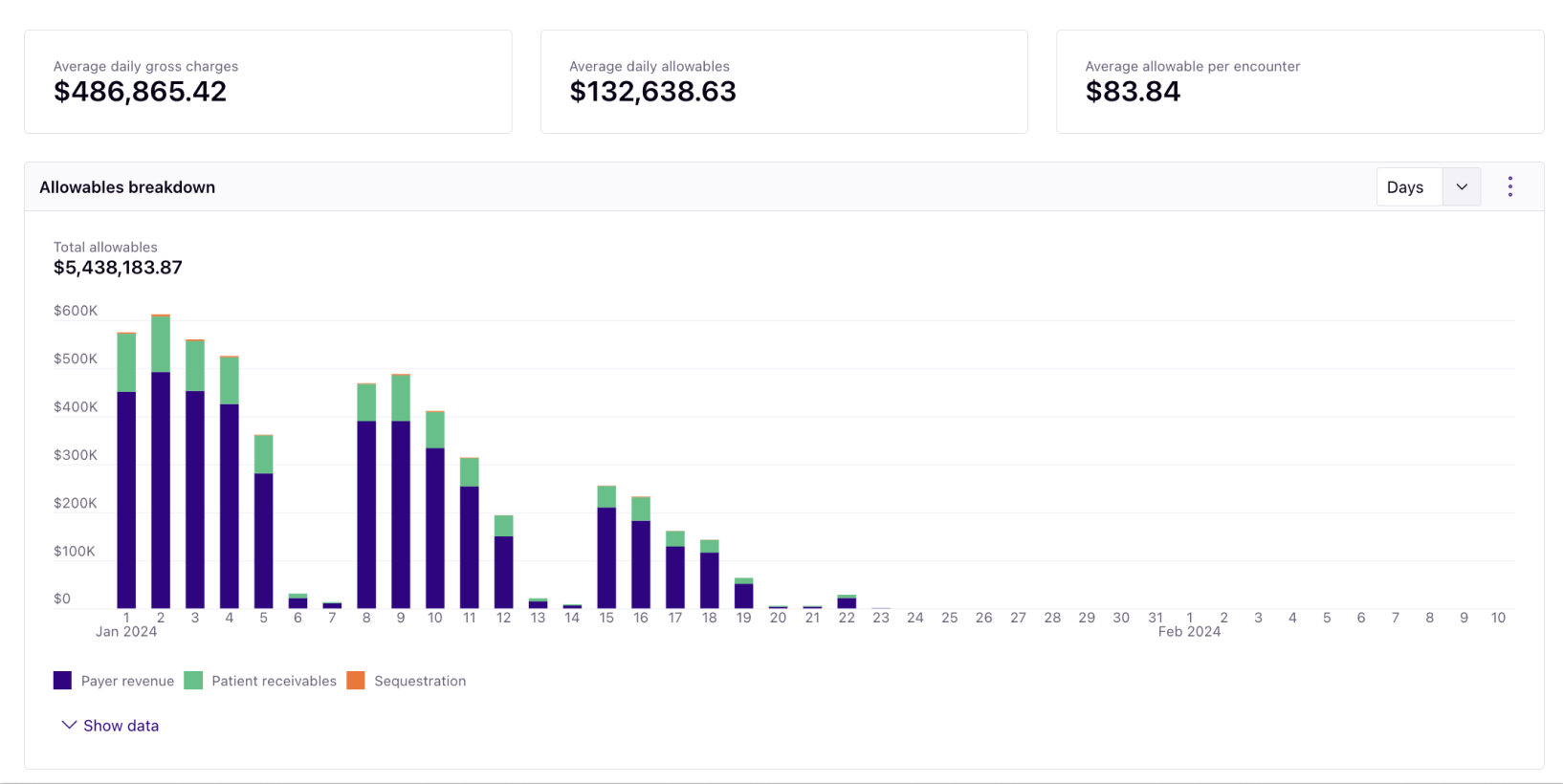
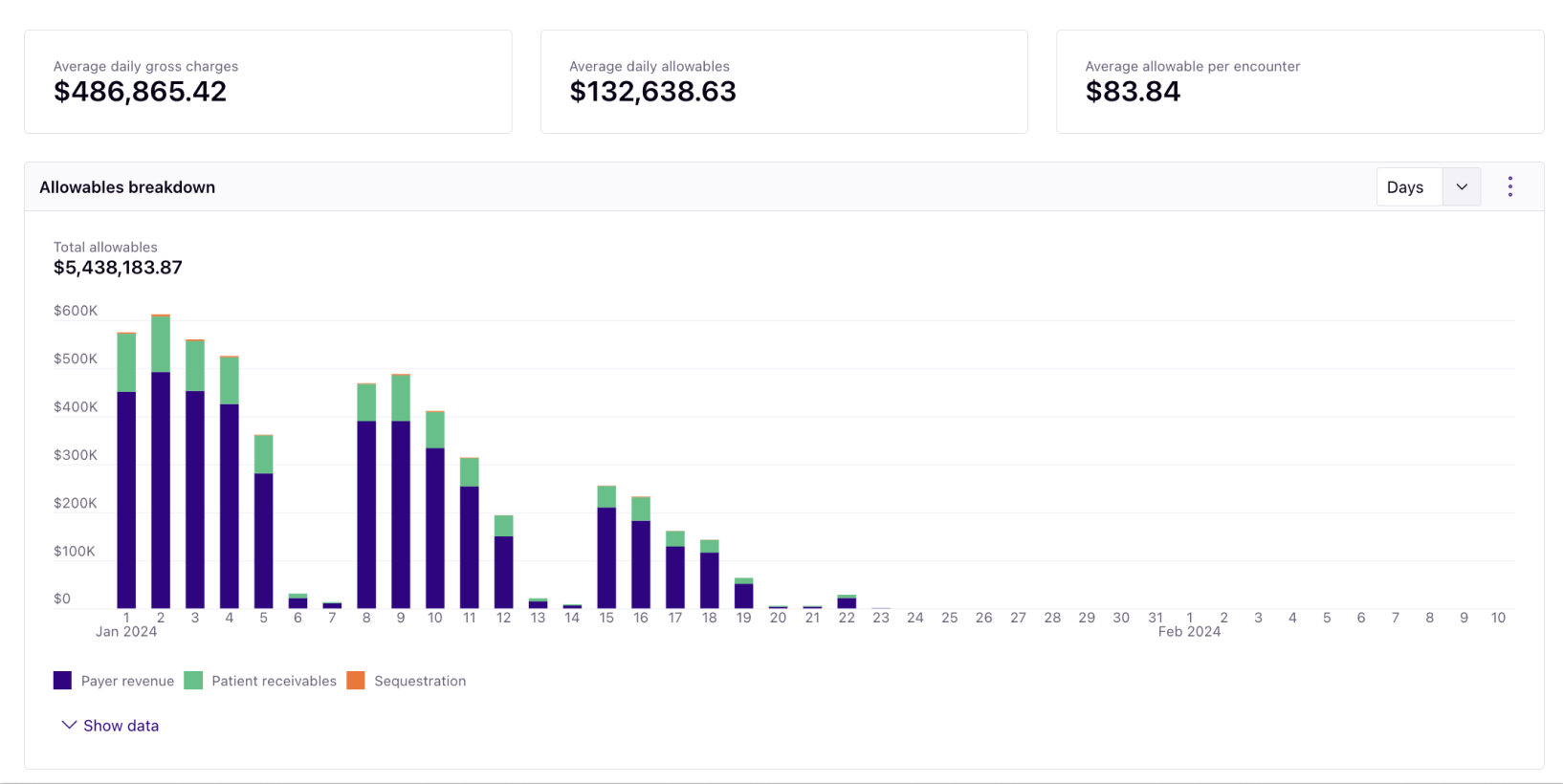

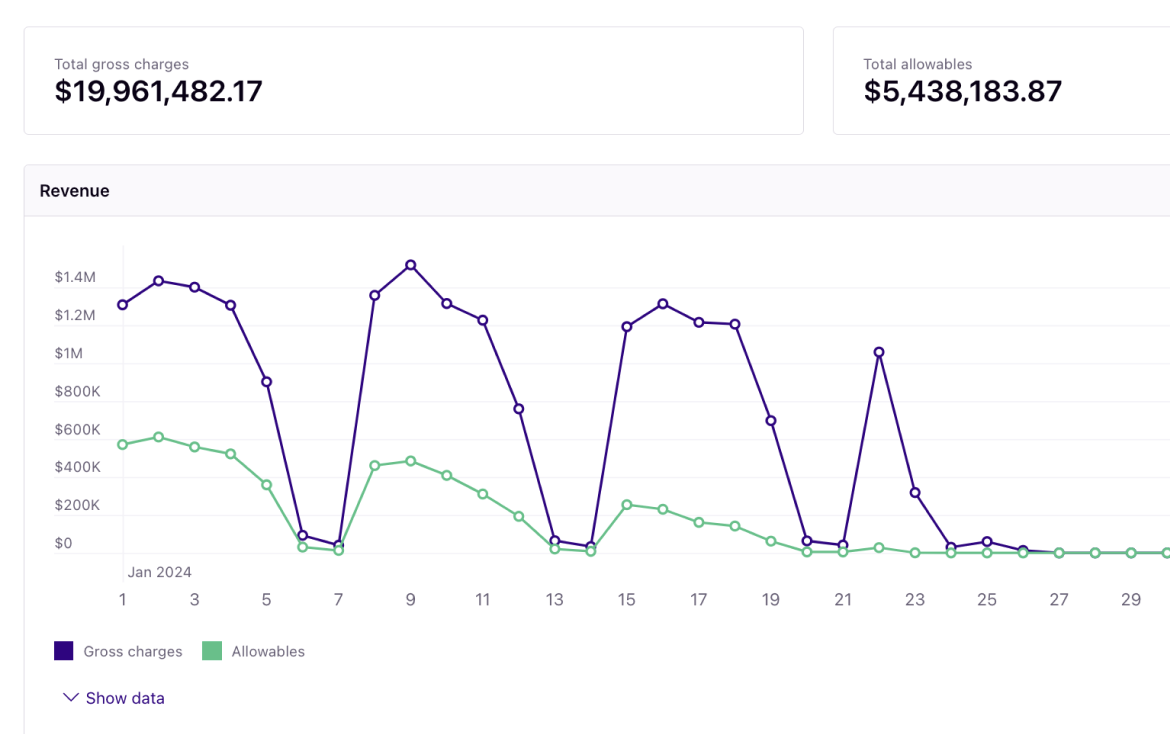
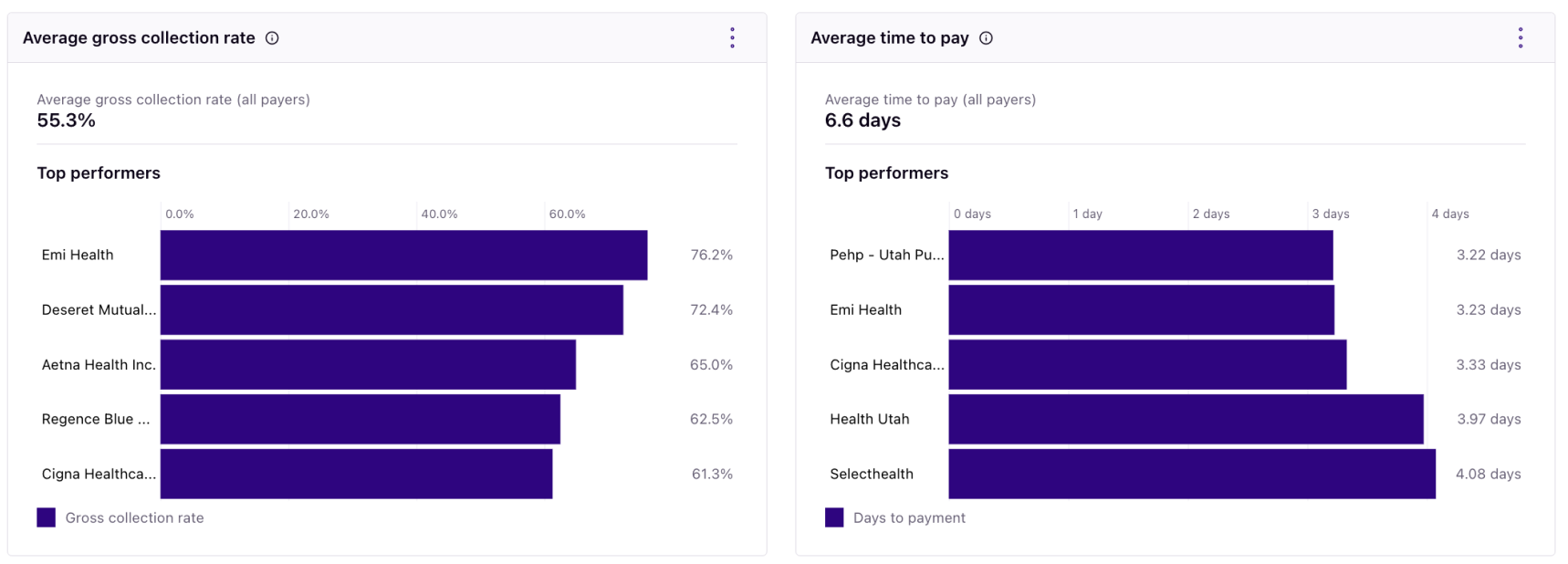
Using your historical and contracted rates as a roadmap, Rivet's RCM solution dives into the trends and nuances needed for a complete picture of what to expect from your revenue. You can capture up-to-date predictions with our management software that allow you to proactively communicate reliable information in your reports — fast.
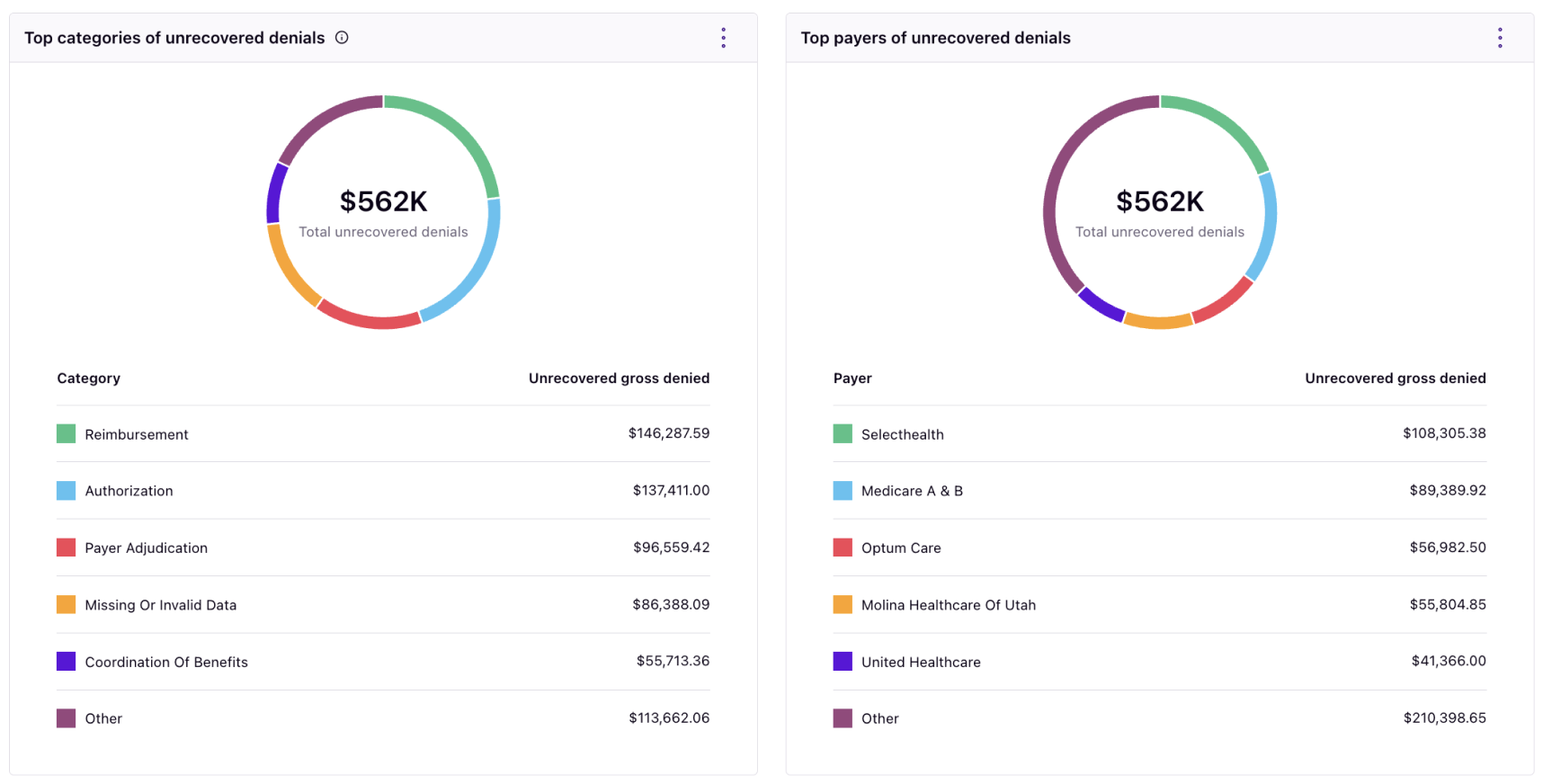

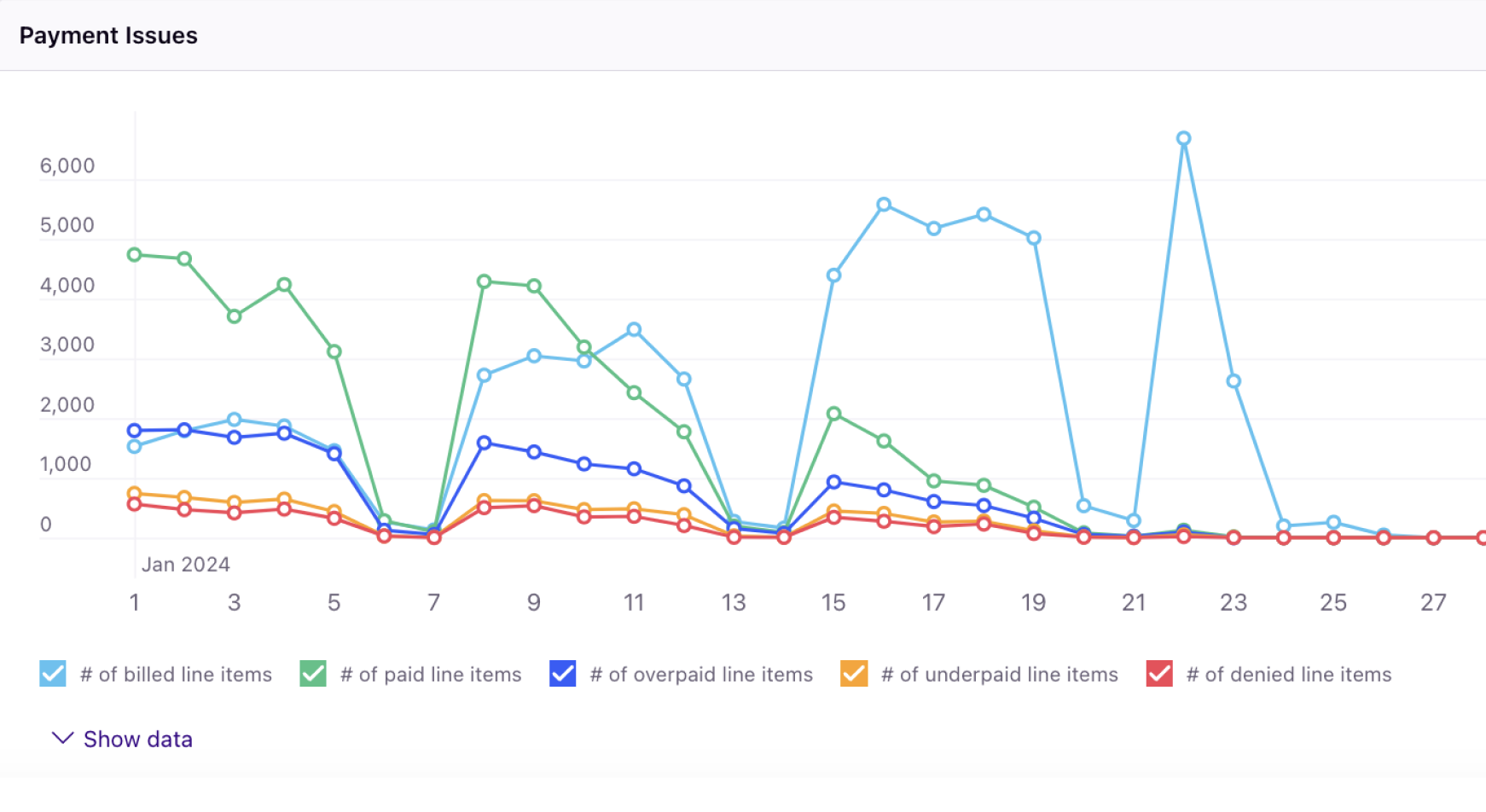
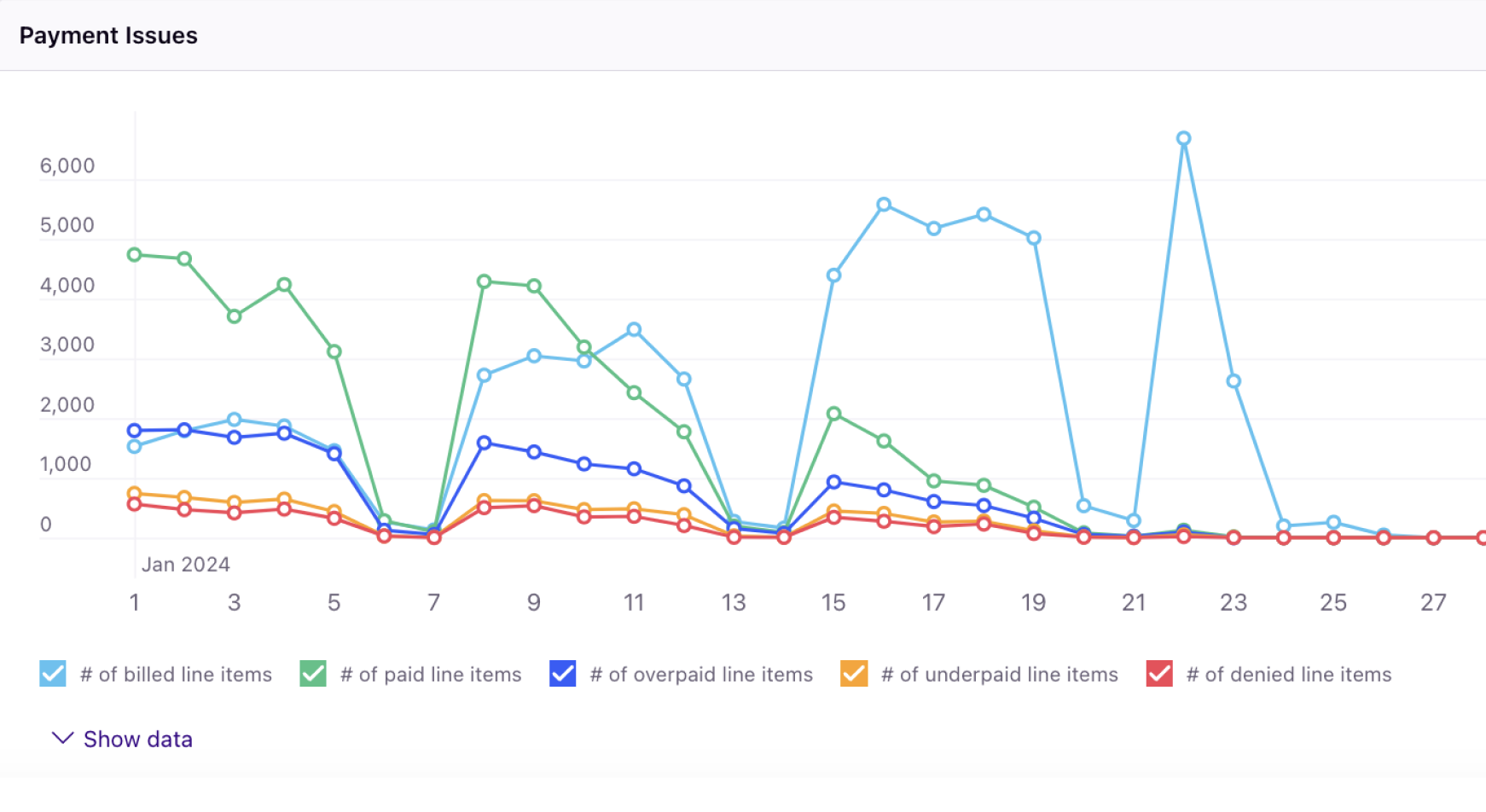
Healthcare organizations' margins are razor thin, so you should spend less time diagnosing revenue leakage and more time increasing revenue through opportunities at your fingertips. Customize how you break down claim adjudication and denied or underpaid claim impact quickly to determine where improvement can be made. And when you do, use the leading denials prevention engine to build better claims.

Empower revenue growth with the data found in your revenue projections, overarching outcome projections, and individual outcome projections. Utilize accurate artificial intelligence algorithmic data to move the needle on revenue and move forward to optimize revenue in the coming months. Forecasting cash and profitability requires confidence. Feel it with Rivet.
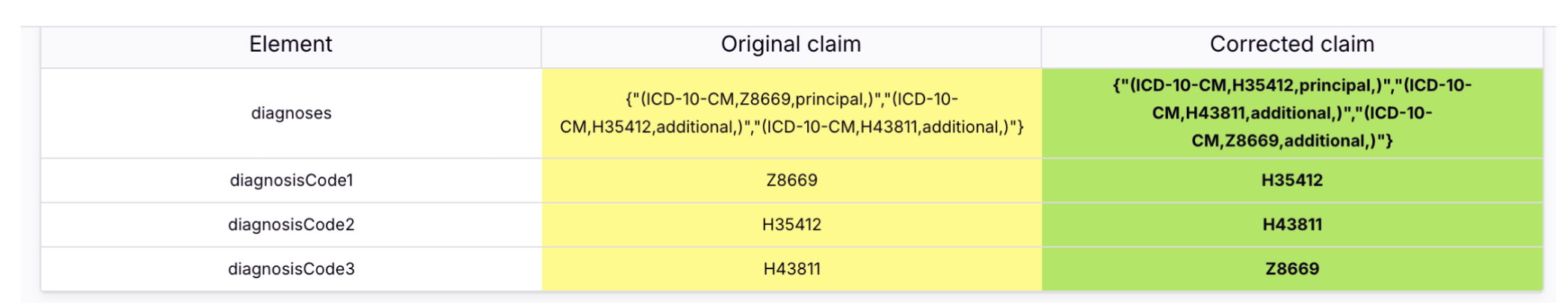
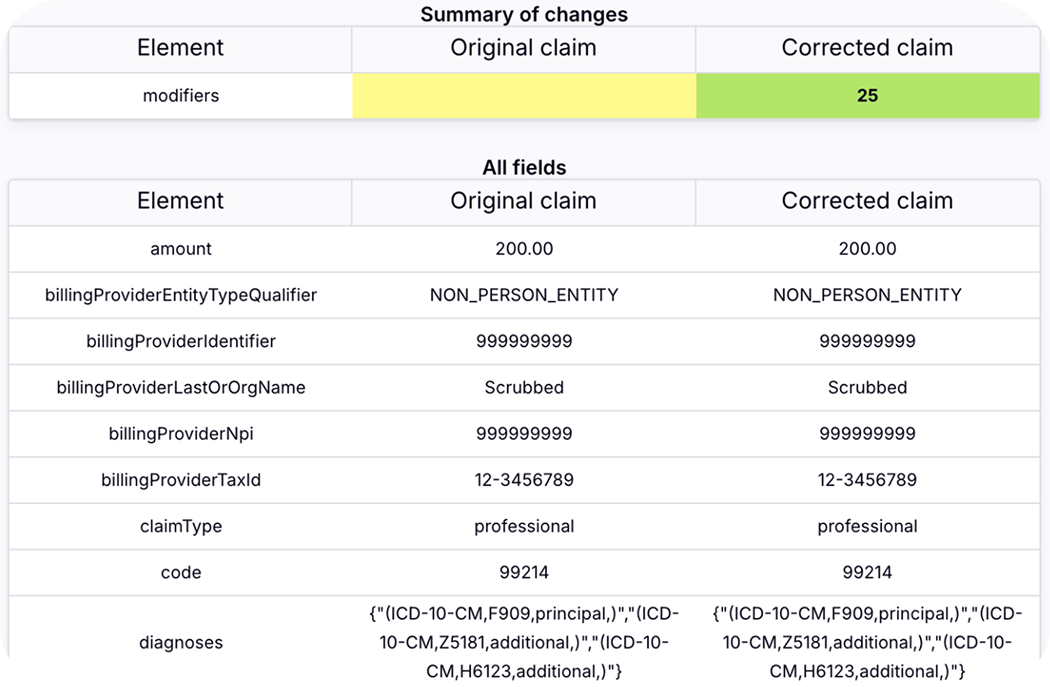
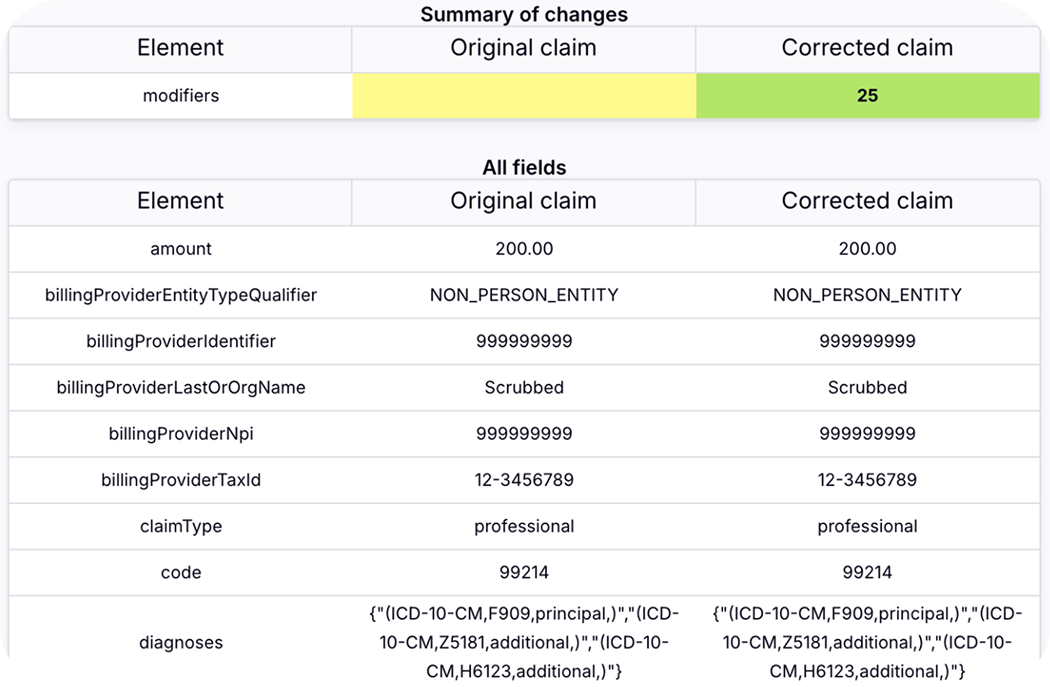
Stop revenue leakage in its tracks with AI-powered billing edits that breakdown diagnosis pointers and allows you to maximize your initial clean claim rate. It's time to fight auto denials with the ultimate denial prevention engine — Rivet.
Rework the denials you do have with ease and speed using Rivet Resolve: the powerful revenue recovery game changer.
“You have to go to the insurance companies’ portals to figure out what’s happening with Every. Single. Claim. Whereas with Rivet, I can click on the claim and it tells me everything I need for rework. After a claim is submitted in our EHR, it takes anywhere from two-to-three weeks before I know about a claim being denied. But in Rivet, I know if a claim is denied within seven to ten days.”
Theresa Mayfield
Revenue Cycle Manager
“We’re so on top of our denials,” she said, “we’re getting claims off of our reports before they can even hit our reports. We’re no longer seeing denied claims become 180+ days old.”
Shantelle Knight
Insurance Processor Services Trainer
“Before Rivet we’d work about 30 appeals a month. I essentially worked about 300 in about 4 days.”
Data Analytics/Informatics Manager
Indiana neurology practice
“Everything I need to work a claim is in Rivet. I can analyze an individual claim without jumping through hoops and going through the payer’s website. It’s all there for me. I can customize my worklist and my team can customize theirs. I work entire lists of denials in Rivet and resubmit claims to payers in bulk. I don’t have to worry about keeping my list up-to-date because Rivet does all the heavy lifting. We’ve saved so much time and energy when it comes to reworking claims. With Rivet, we’re working smarter, not harder.”
Angela Phillips
Medical Billing Specialist


Healthcare Revenue Cycle Management (RCM) software simplifies and streamlines the billing and financial process for healthcare providers. It automates key steps like denial management, patient billing, error reduction and efficiency improvement. Rivet is a healthcare RCM software that leverages AI technology to offer denials prevention, payer contract comparison and management, reimbursement key performance indicator (KPI) reports and analytics, underpayment detection and workflows, patient cost estimates with insurance eligibility verification, and pre-collections management.
Healthcare practices need software additional to their Practice Management (PM) system or Electronic Medical Records (EMR) platform to effectively manage revenue cycle operations because cost margins are slim and overhead cost is high. Healthcare Revenue Cycle Management solutions ensure accurate billing, efficient claim management, and proper reimbursement from patients and payers. Efficient RCM solutions should also provide revenue integrity (such as denials management and prevention), optimize contractual reimbursement from insurance payers, and enable practices to focus on patient care.
Advanced revenue cycle management software (Rivet) provides dashboard visuals and analytics to dive into your Key Performance Indicators (KPIs) which focus on key areas like revenue cycle management and profitability. Each KPI can be looked at for a set amount of time such as a month, quarter, and year.
Financial health is measured through KPI criteria such as the following:
Process large volumes of financial and operational metrics with Rivet healthcare revenue analytics and revenue cycle management software. Revenue managers easily execute financial strategic initiatives by first auditing and analyzing complex historical, real-time, and projected revenue in Rivet. Then managers review and pivot as needed in seconds with empowered, HIPAA compliant, AI-driven technology. Use automation for charts and tables to get both a bird's eye view of operations as a whole, with the capability to focus data all the way down to specific claims to uncover trends with denials, underpayments, claim volume, payer mix, etc.

