

Healthcare reimbursement is complex. With limited time and resources for claims review, your practice is likely experiencing payment discrepancies that affect your bottom line.
In the end, you're losing out on revenue. You need a system to cull and manage your contracts and fee schedules and help you know where your rates stand against others in your area.
Without a contract watchdog, you're leaving money on the table.

Good thing Rivet can help you find not only your footing on payer contracts, but also help recover your money: fast. We build a solid foundation for you; centralizing your payer contracts like a backbone for your billing workflows.
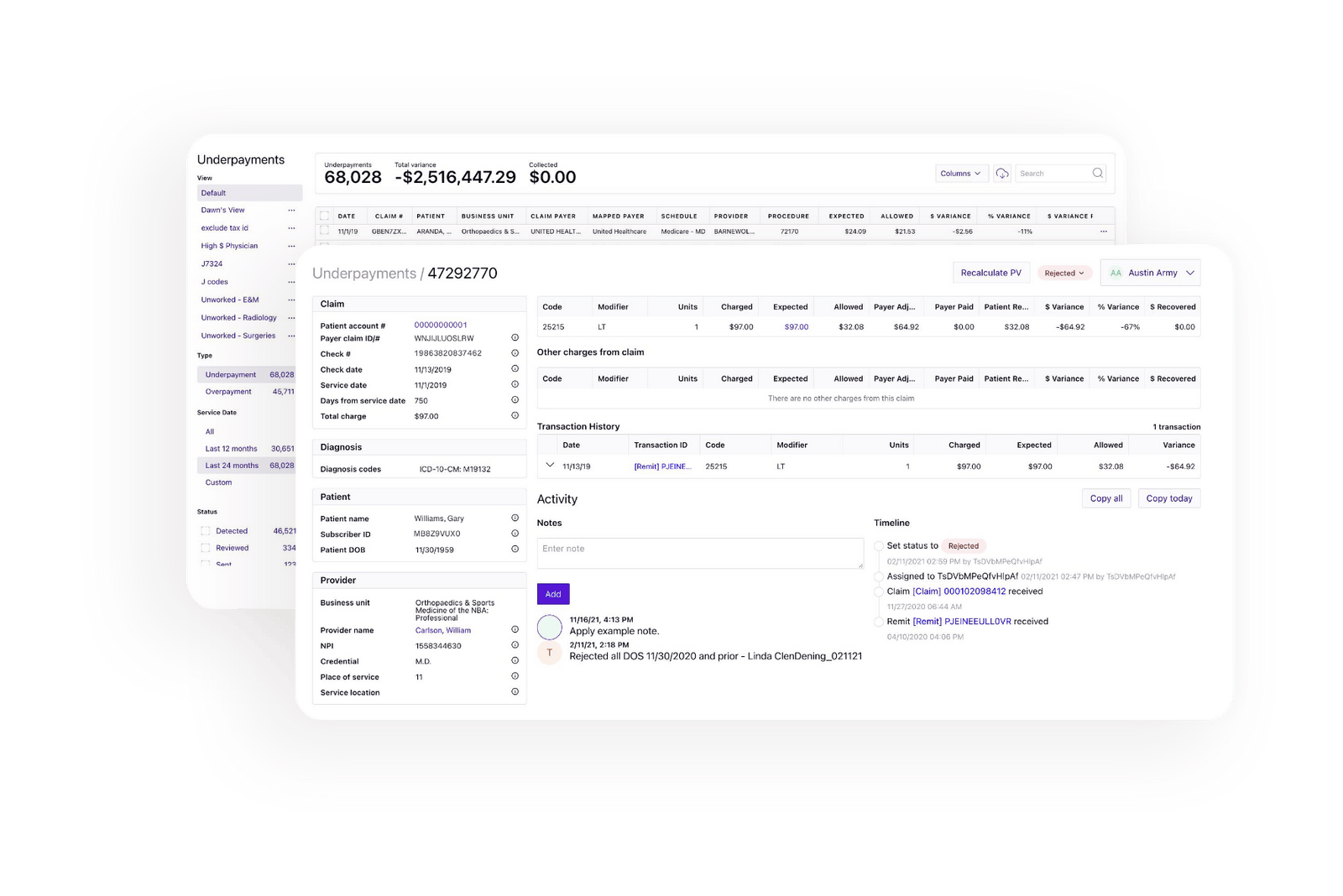
With it all in one place, you can model the best terms for a new contract, compare payers to optimize reimbursement and assess claims analytics to gain key insights on your claims, your revenue, your pricing, and what money needs rescuing.
.png)
.png)
.png)

.png)



AI algorithms bring your payer contract data together to unlock the knowledge you need to fuel your business and your accounts receivable. With the right information at your fingertips and an easy way to make sense of it — you’re ahead of the curve that you did not know you could ever straighten out.

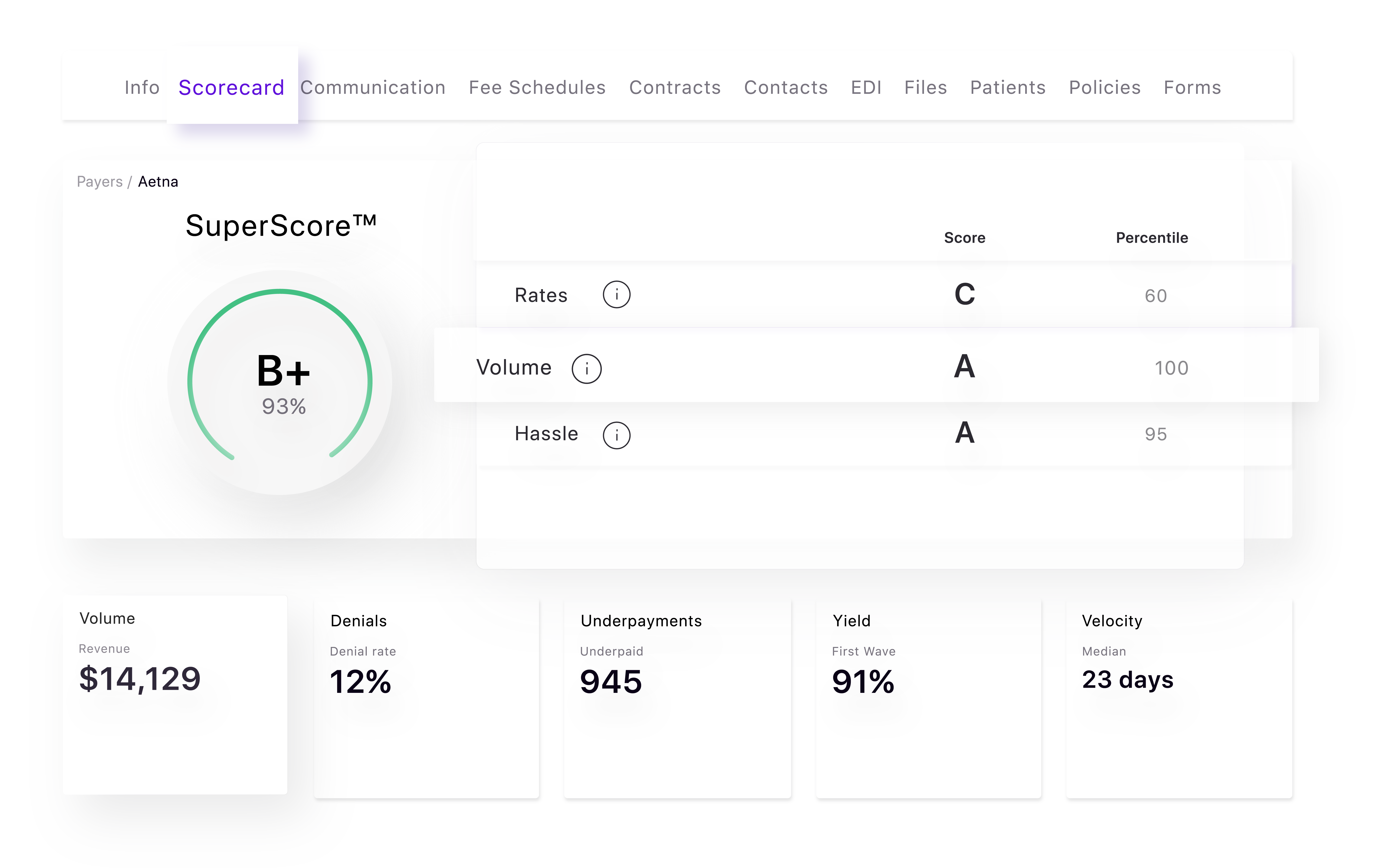
With a strong centralized data brain performing at its peak to help you recognize your revenue potential — Rivet delivers the must-have tool every healthcare organization needs to review payer rates compared to local competitors. The contract management process also allows you to assess, manage and negotiate contract needs to make the most out of every clause in a contract, from escalators to rates and everything in between that can make you the business success story you deserve to be.

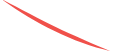
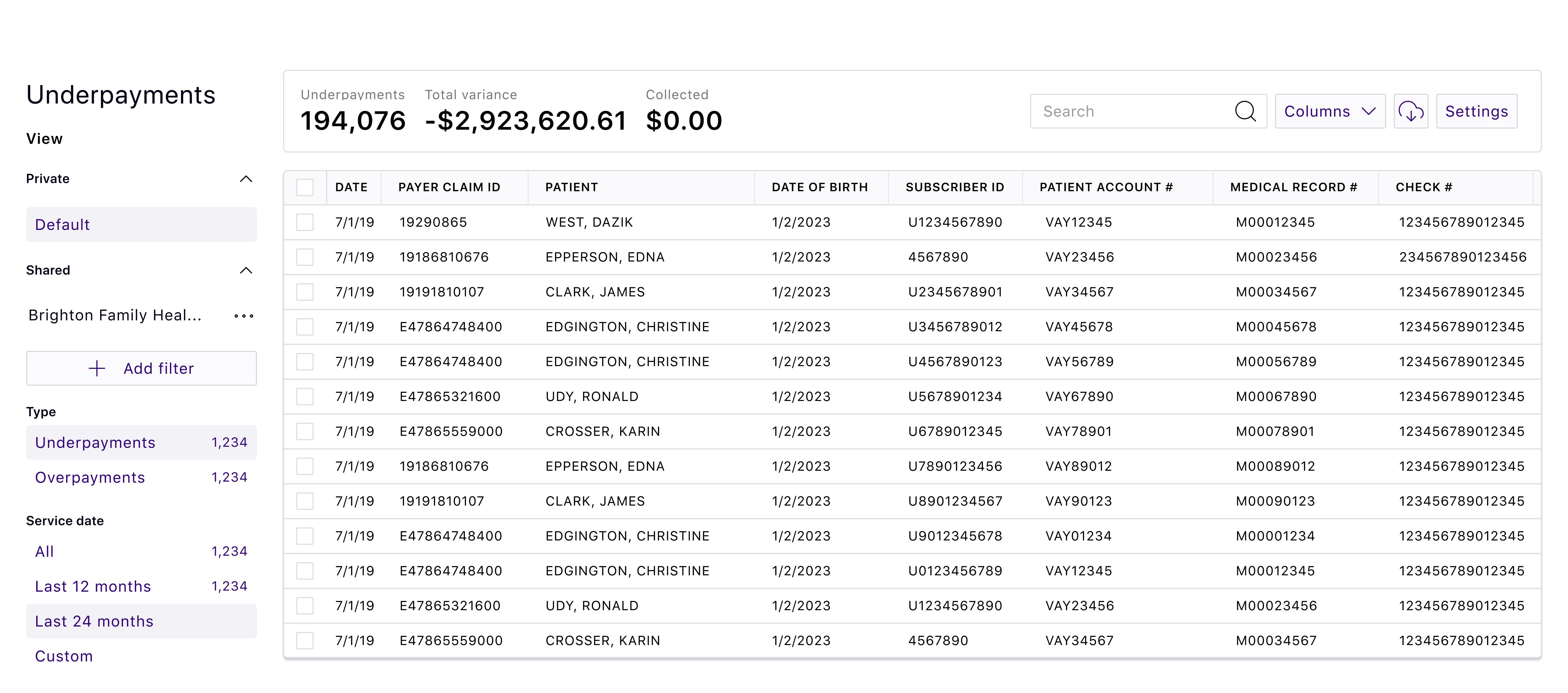
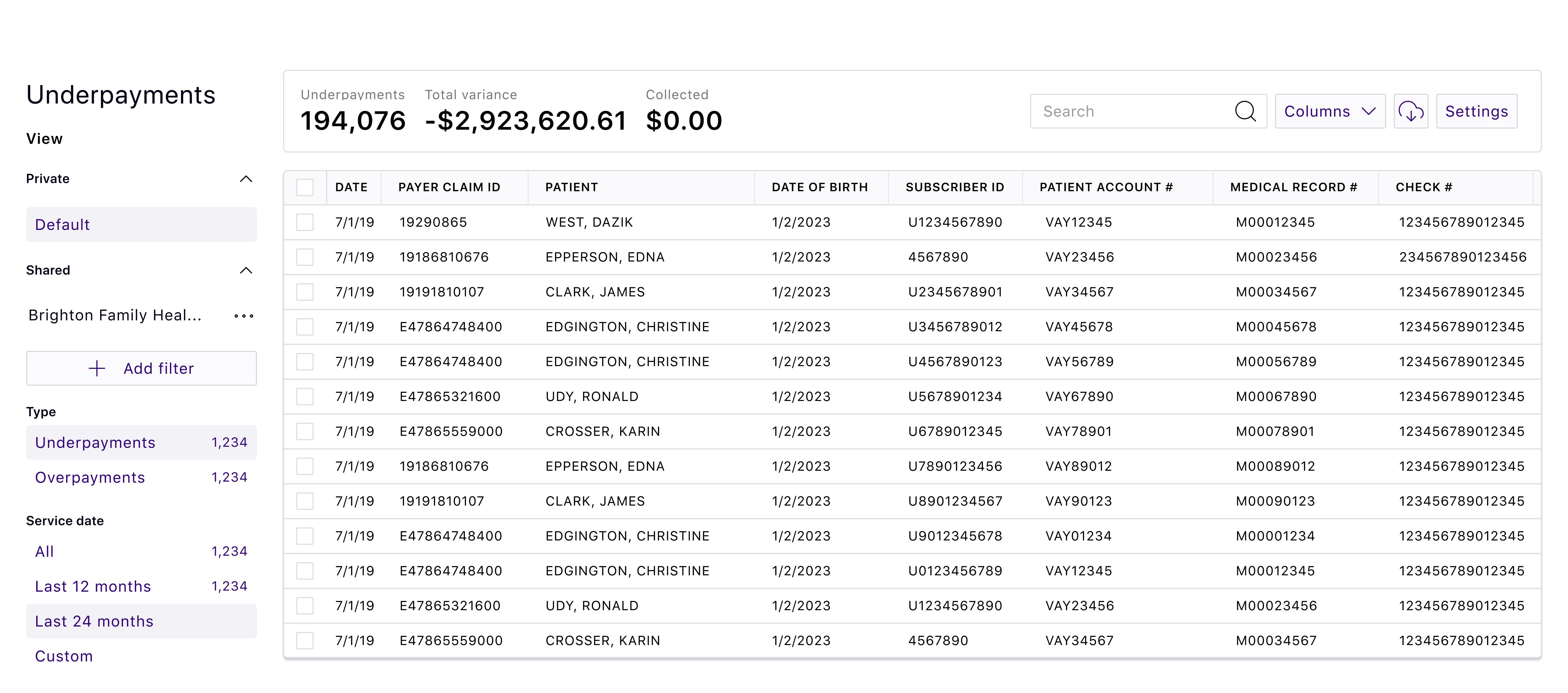
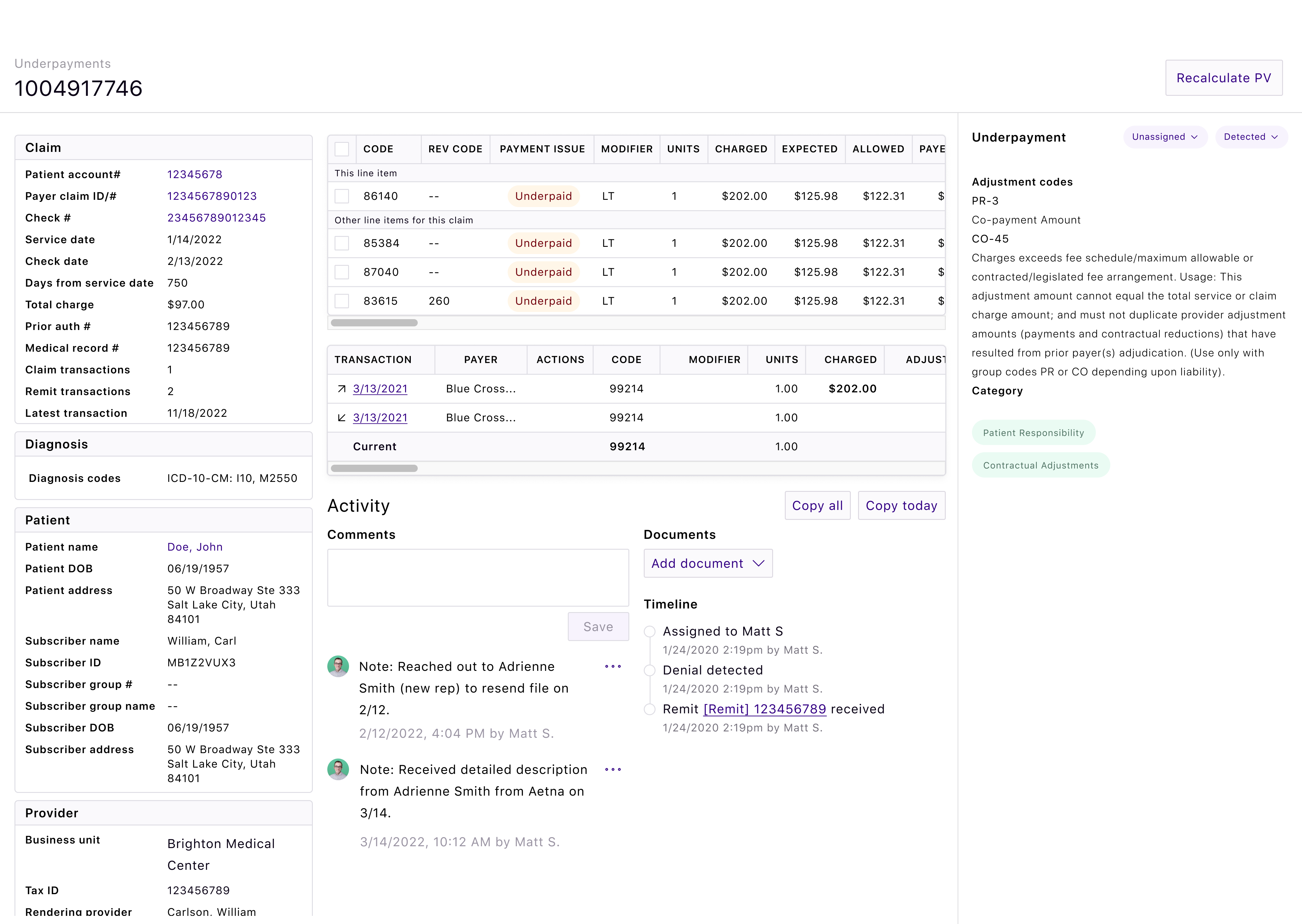
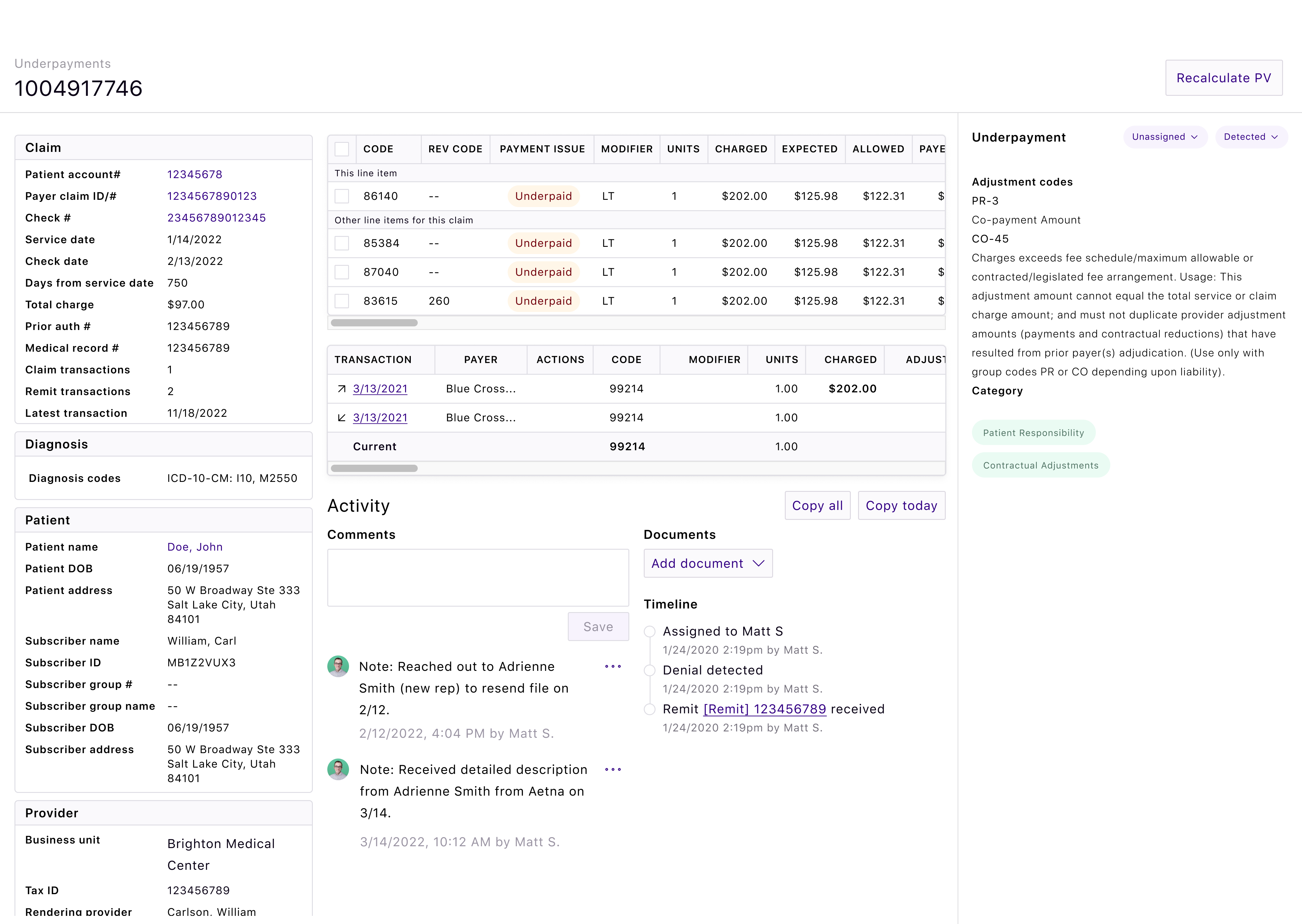
Rivet turns on the light in your reimbursement black hole by auto-detecting and reporting on payment variances — faster than most revenue cycle management systems. Knowing where to dig for gold is only the first part of the equation. We also offer the easy-to-use platform on which to recover your revenue and resolve systemic submission issues with validation logic to correct future issues.
“I just fell in love with the underpayments solution. I loved the analytics piece, the reporting, that it was so easy to use, that you could drill down different ways, and that it integrated with our practice management system. I knew this is what we had to do and it’s been a great investment for us. ”
Tonia Bateman
Business Office Director
“ It's been a really great tool to maintain our contracts and identify underpayments. It's nice that everything lives in one place, and I'm not going all over to find what I need or opening all these different spreadsheets. I have one central tool that I can track and monitor payments and move them into worklists depending on their completion status. The current list of underpayments I’m working on will pay for the tool by itself and that’s huge.”
Travis Seymour
Contract Management Specialist
“With how quickly Rivet responds [an average 30 seconds wait time!] we feel like their team is right in our office.”
Kellie Ickowski
Practice Administrator
“Medical contracting is like the biggest black box. It’s confusing on our side as the providers, and it’s confusing on the payer’s side as they adjudicate claims. There is no way to know how well your contracts are performing without a tool like Rivet. The analytics and data aggregation tools in Rivet are great: we can sort and display claims data in ways you’d never be able to do on your own. It’s awesome. Rivet’s software is a necessity to manage medical practices of any size.”
Peggy Harris
Chief Financial Officer
“Everything I need to work a claim is in Rivet. I can analyze an individual claim without jumping through hoops and going through the payer’s website. It’s all there for me. I can customize my worklist and my team can customize theirs. We work on our own lists and even assign one another to a claim we’re working on, just to get a second pair of eyes on the claim. ”
Angela Phillips
Medical Billing Specialist


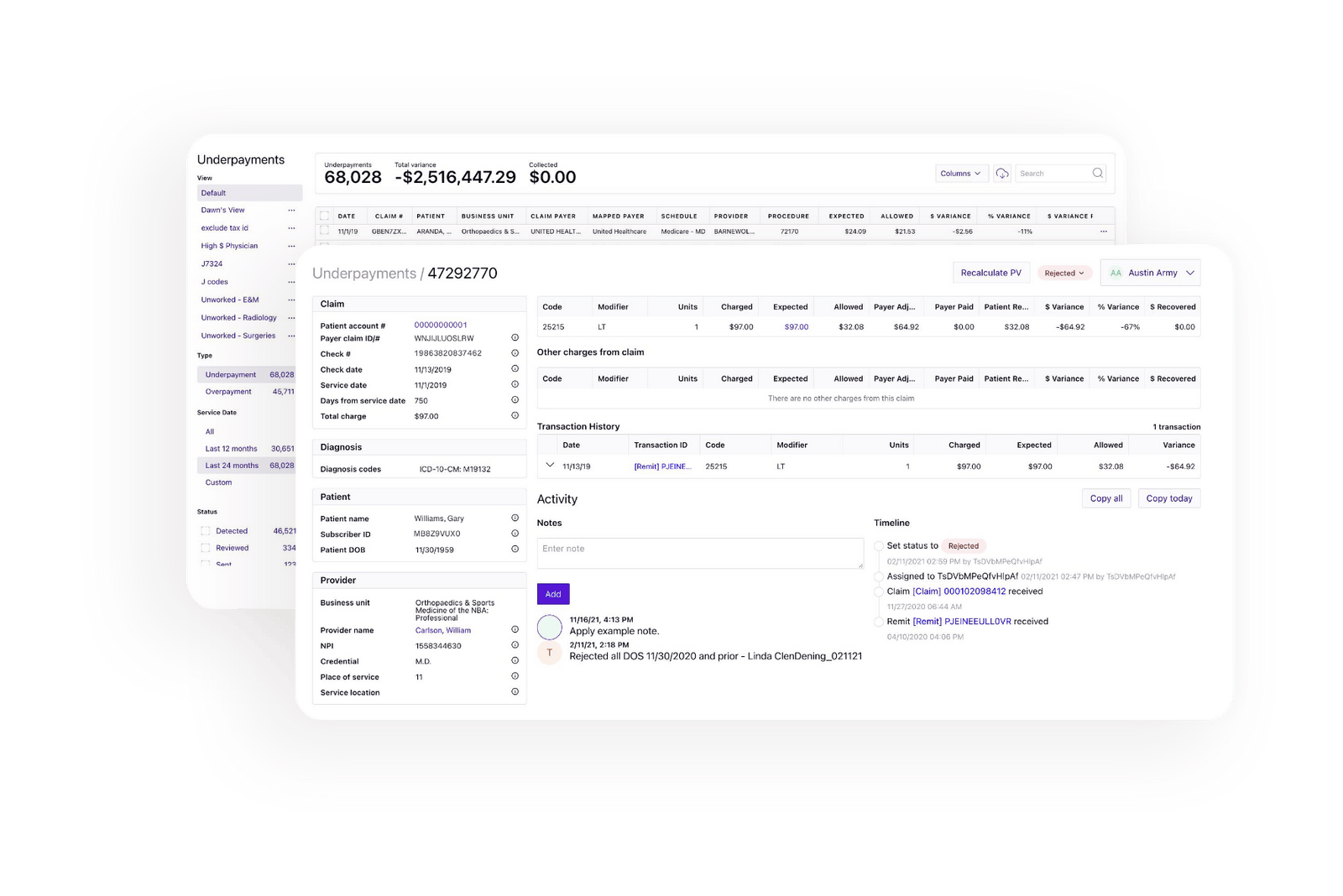
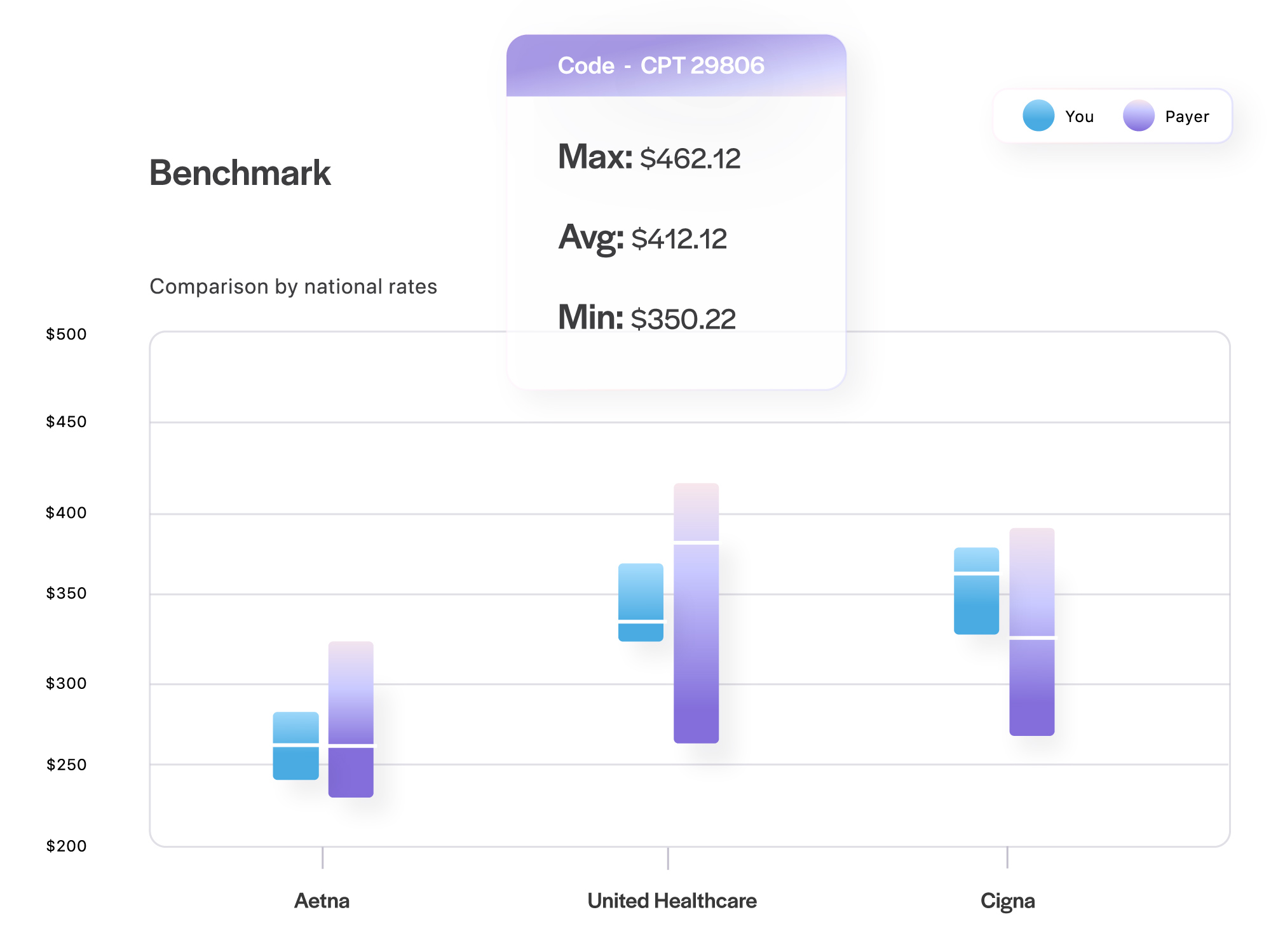
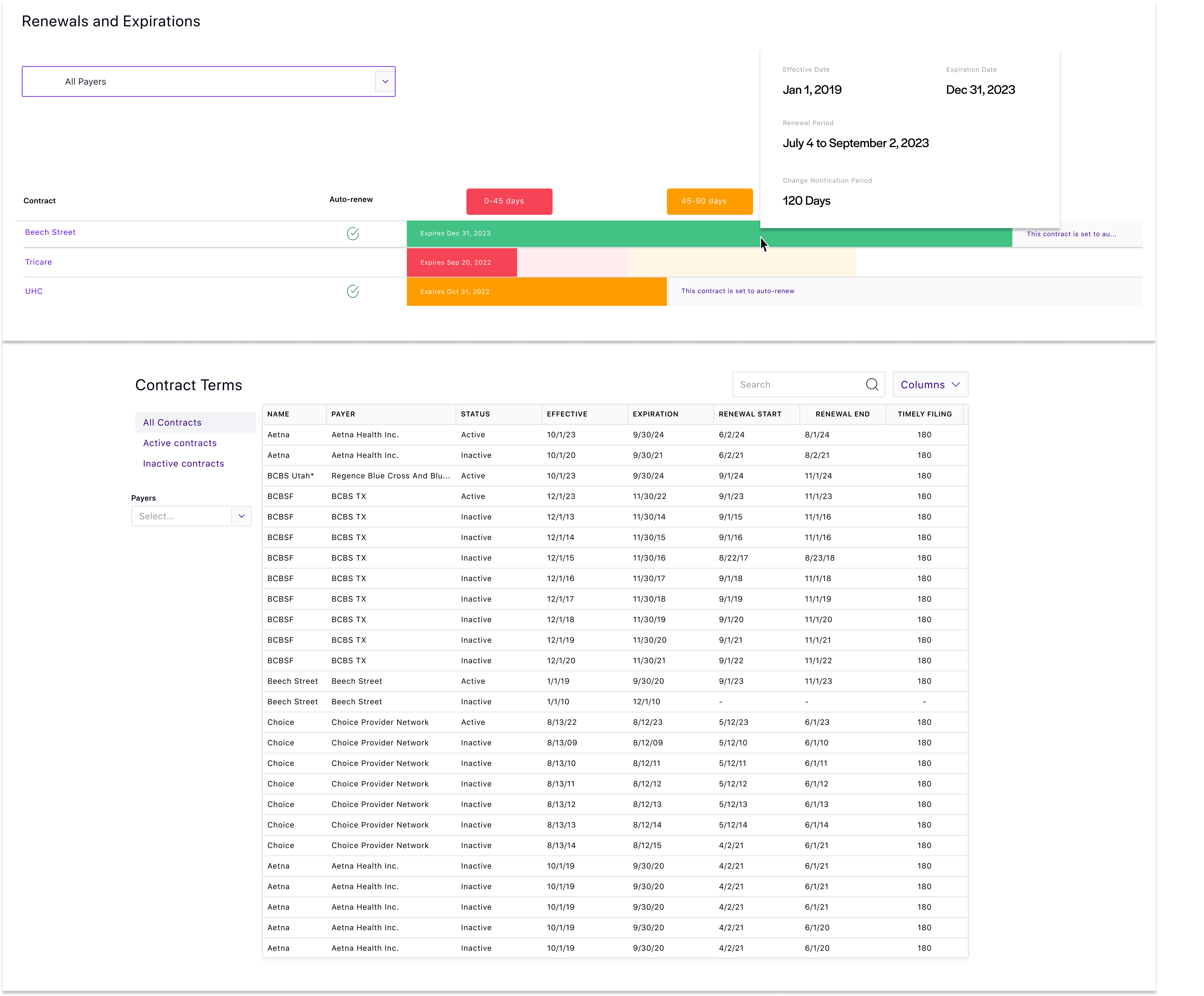
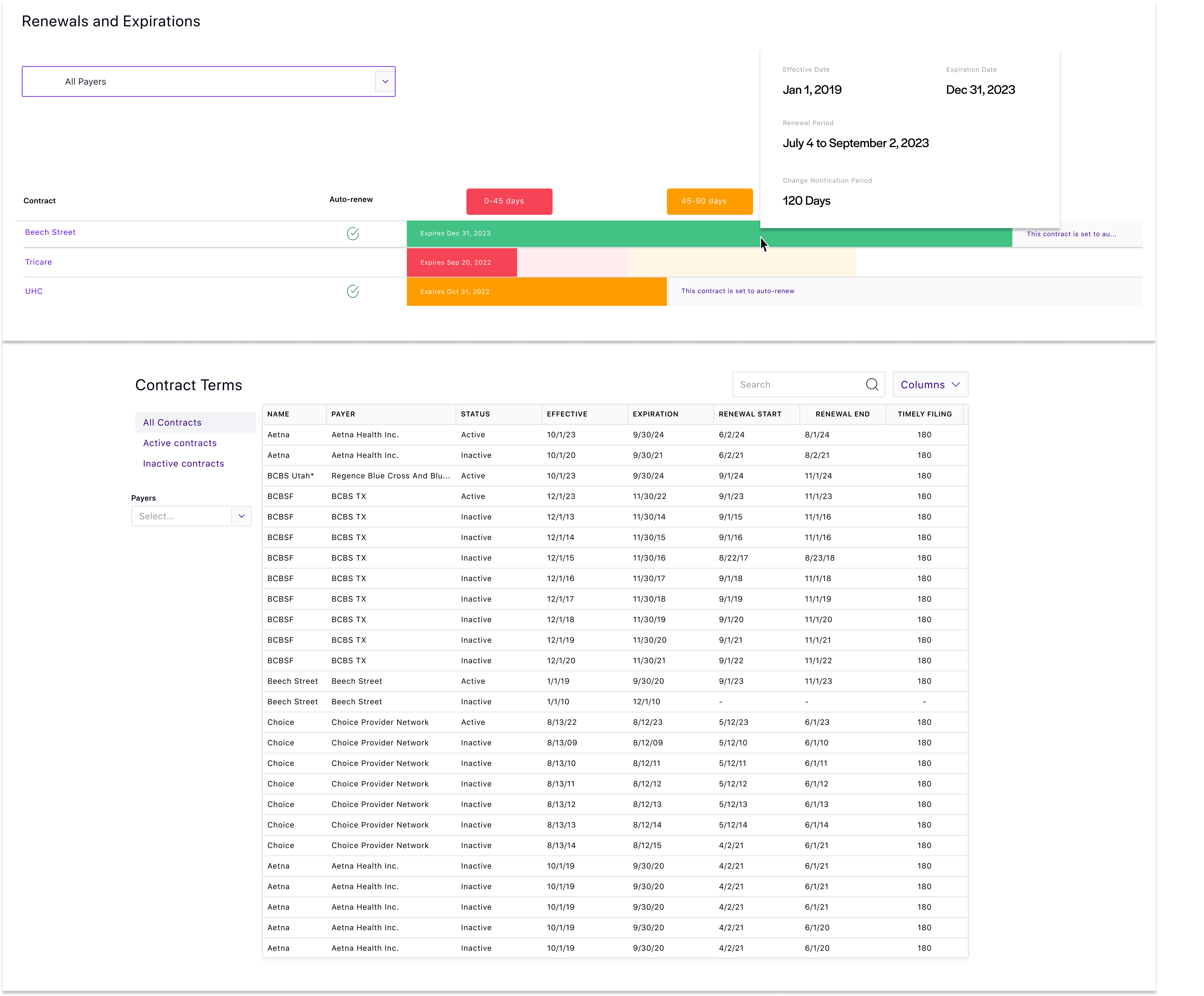
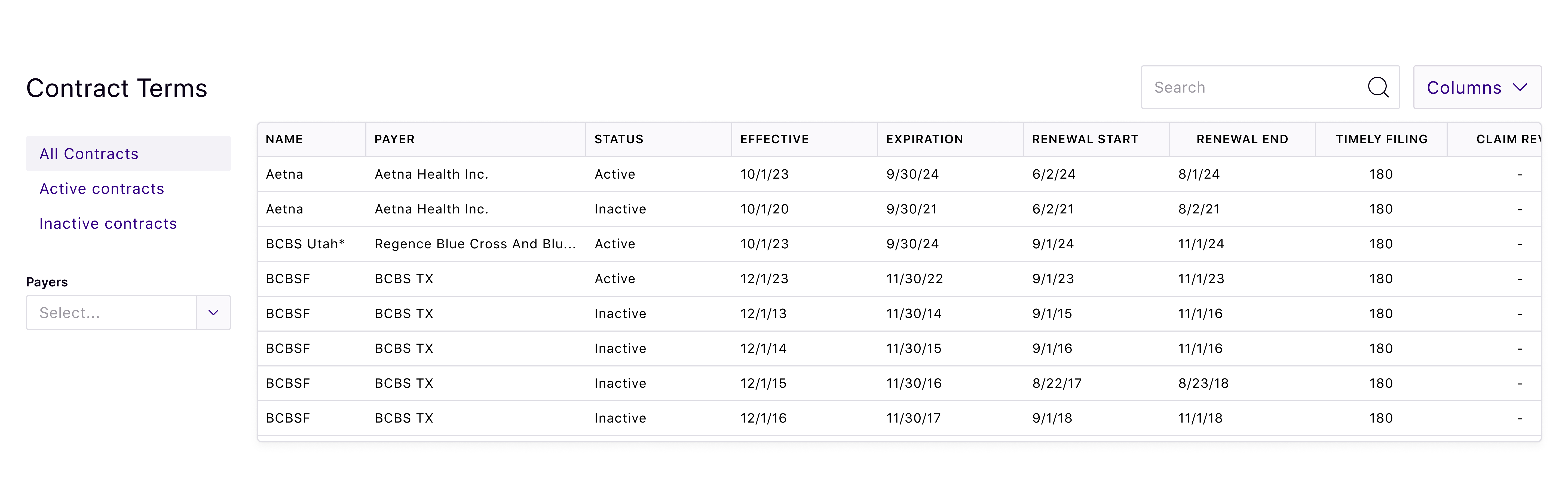
Rivet payer contract management software maintains contract terms and agreements, audits claims for improper payment, optimizes provider charge pricing, analyzes contracts against proposed changes, and compares contracts to providers and insurance carriers anywhere in the U.S. Gain a centralized location for all contracts to track renewal timelines and prepare for upcoming negotiations or new contracts. Compare contracts to each other in seconds for maximum payer contracting efficiency.
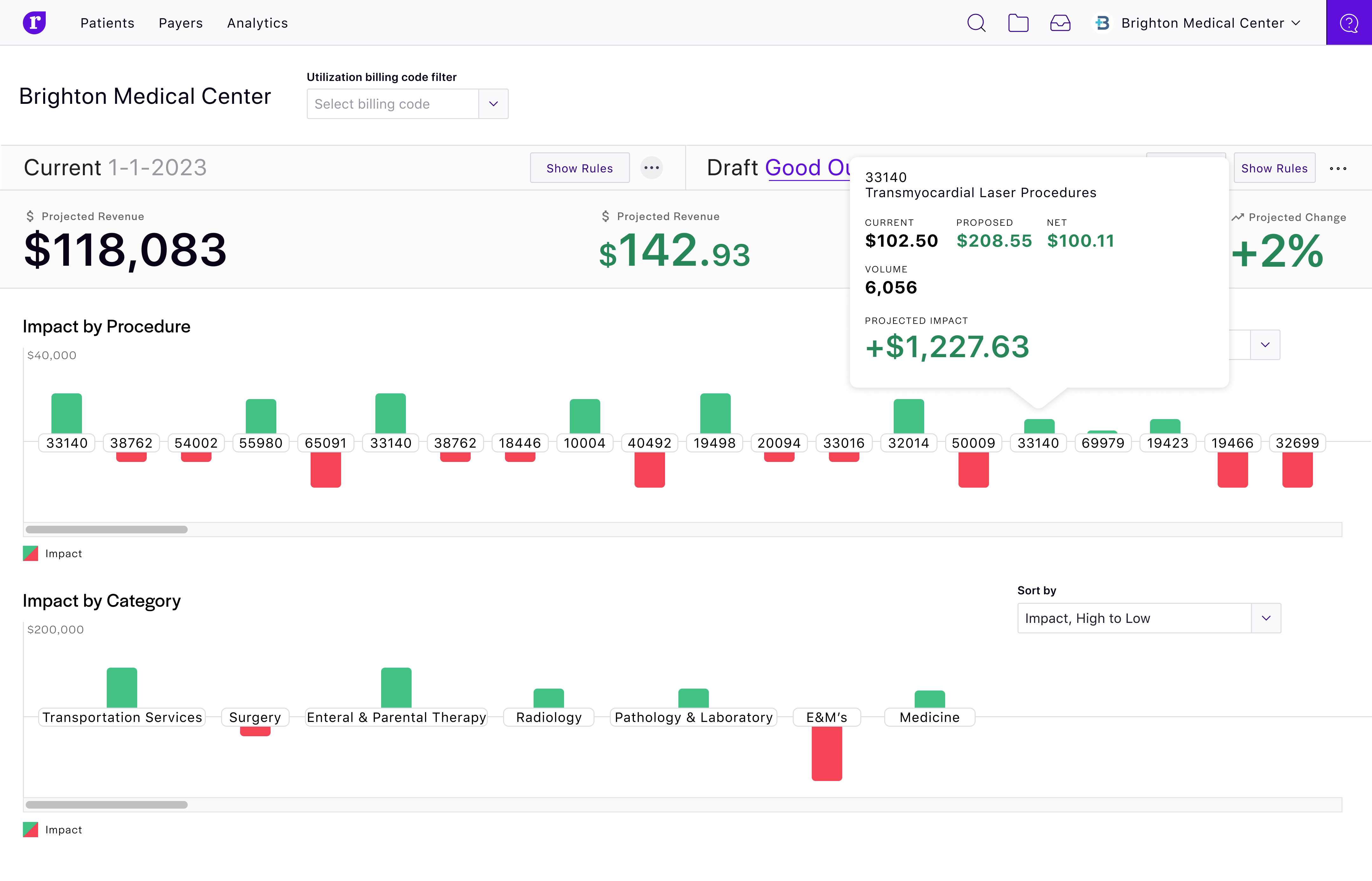
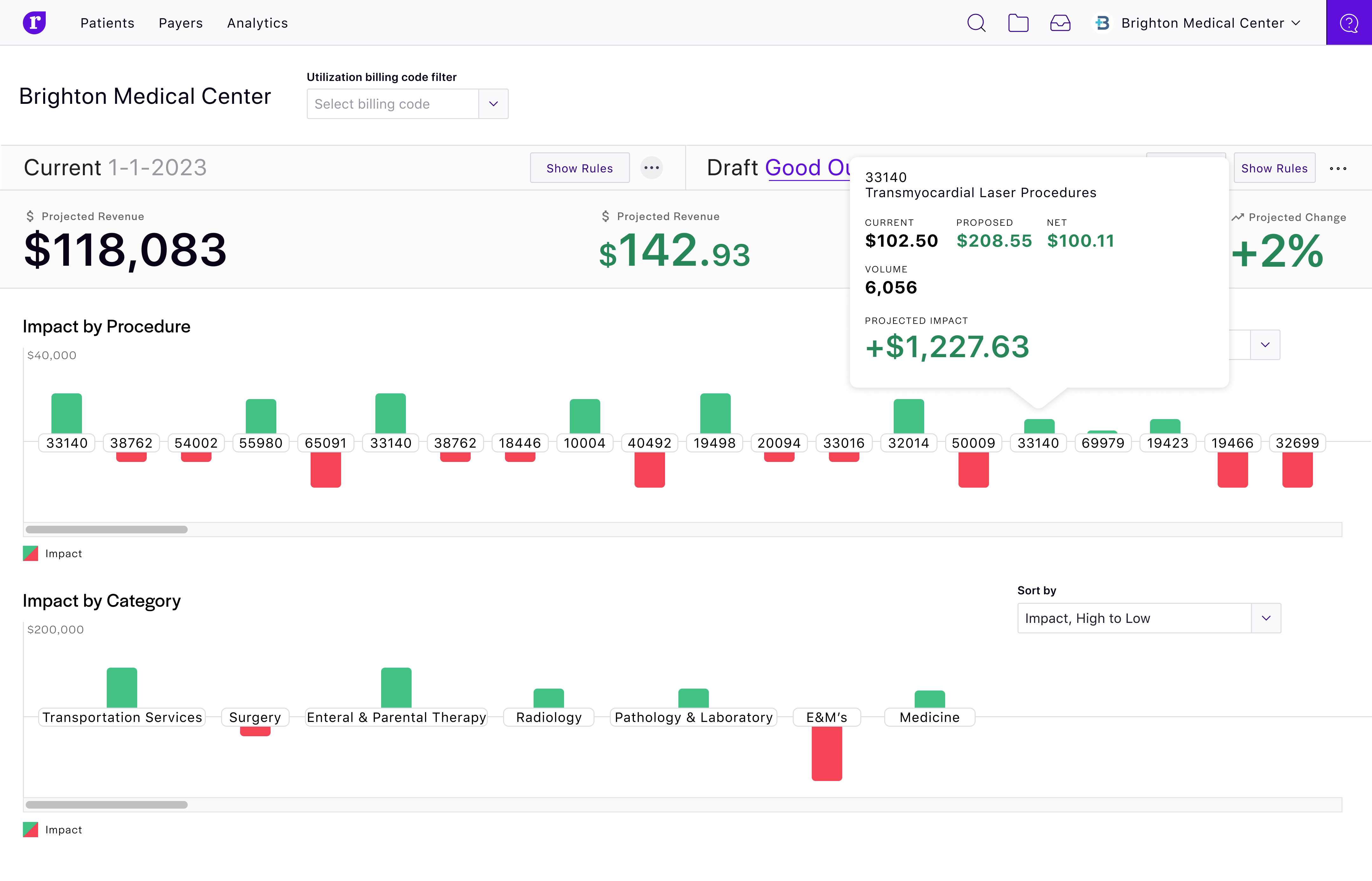
For upcoming payer contract renewals, Rivet manages negotiation/renewal timelines to know when to prioritize a specific contract, models proposed contract changes and compares rates to previous contracts with the same payer or a practice’s other contracts, contrasts a practice’s current rates with every other healthcare provider across the U.S., and analyzes key performance indicators (KPIs) to allow for payer contract negotiation fodder.
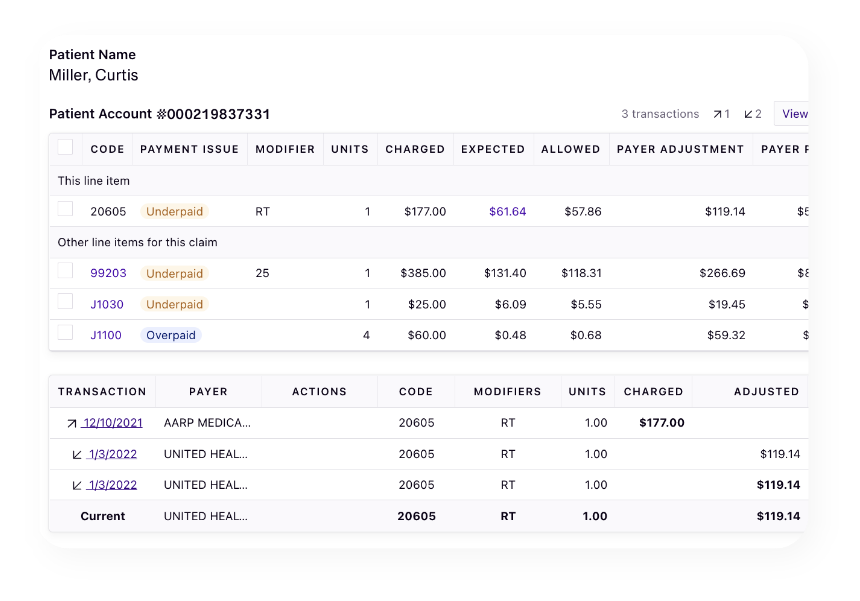
Underpaid claims are best recovered in a project with several similar claims attached. Rivet audits all claims and groups similar underpaid claims into projects and then estimates the value of each project for simple prioritization. Rivet payer contract software offers the proof needed to fight the battle of improper insurance payment. All underpayment projects in Rivet are downloadable in CSV format for easy insurance send.

